
THE PARAMEDICS radioed in the details to the rural Ontario hospital: female teenager, intentional overdose, ETA five minutes. The patient’s mother arrived with her, wearing a look I had grown all too familiar with — bewilderment, incredulity, fear. When I’d taken the job as an emergency- department clerk, I’d steeled myself for blood and guts, for car accidents and broken bones. But I wasn’t prepared for the sheer number of cases like this one.
After the girl was out of medical danger, the emergency physician asked me to contact the attending psychiatrist, who would speak with the girl and try to find out what had triggered her suicide attempt. Beyond this consultation, however, the patient and her family would be largely on their own, left to navigate a fragmented system that has allowed too many young people to fall through the cracks.
Last June, researchers from the Children’s Hospital of Eastern Ontario, the University of Ottawa, and McGill University released a study about emergency-department visits by Ontario adolescents between 2003 and 2017. Beginning in 2009, the number of adolescents presenting for self-harm increased sharply, more than doubling between then and 2017. Visits for mental health issues, such as anxiety, depression, and suicidal ideation, rose 78 percent over the same eight-year period. Mental health professionals report children as young as seven or eight expressing a desire to take their own lives.
Across the country, the situation is similarly dire. In BC, almost one in five of the province’s students reported having seriously considered suicide in the past year, according to a survey by the youth health nonprofit McCreary Centre Society. And, according to Judy Darcy, BC’s minister of mental health and addictions, Indigenous youth in the province are dying of suicide at a rate four to five times higher than their non-Indigenous peers.
This story is from the November/December 2020 edition of The Walrus.
Start your 7-day Magzter GOLD free trial to access thousands of curated premium stories, and 8,500+ magazines and newspapers.
Already a subscriber ? Sign In
This story is from the November/December 2020 edition of The Walrus.
Start your 7-day Magzter GOLD free trial to access thousands of curated premium stories, and 8,500+ magazines and newspapers.
Already a subscriber? Sign In

Invisible Lives
Without immigration status, Canada's undocumented youth stay in the shadows

My Guilty Pleasure
"The late nights are mine alone, and I'll spend them however I damn well please"
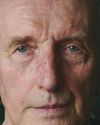
Vaclav Smil Is Fed Up
The acclaimed environmental scientist is criticizing climate activists, shunning media, and stepping back just when we need him most

It's Time for a Birth Control Revolution
What the pill teaches us about the failure - and future - of women's health care

Would You Watch a Play about Hydro Electricity?
How documentary theatre struck a chord in Quebec

Still Spinning
One record chain has bet big on a new appetite for physical media

Just So You Know, I Love My Mother
In many ways, multi-generational living makes sense. But that doesn't make it easy

Art of the Steal
Why are plundered African artifacts still in Western museums?

Canada in the Middle
What role can we play in easing the war in Gaza?
Canadian Multiculturalism: A Work in Progress
As we mark fifty years since the adoption of Canada’s federal multiculturalism policy, human rights advocate AMIRA ELGHAWABY celebrates its merits and reflects on the work that is yet to be done when it comes to inclusion, acceptance, and fighting systemic racism in our country.