
WORD OF MERCY HOSPITAL’S DEMISE BEGAN TO circulate just after 9 a.m. on July 29, 2020. The hospital’s chief executive officer summoned the medical executive committee to an unscheduled conference call. She told them she’d be sending a staff-wide memo shortly and felt a heads-up was in order.
“The decision to discontinue services at Mercy Hospital was not an easy one,” the memo read. More words followed— something about decreasing hospital reimbursements and ballooning capital expenses. Dr. Adele Joy Cobbs, an emergency physician on the committee, felt blindsided. She listened to the reactions of the other committee members on the call. The seconds ticked by.
“There was absolute silence,” Cobbs recalled afterward. “Not a word from anyone. It just reflected the disbelief.”
This story is from the October 04, 2021 edition of Bloomberg Businessweek.
Start your 7-day Magzter GOLD free trial to access thousands of curated premium stories, and 8,500+ magazines and newspapers.
Already a subscriber ? Sign In
This story is from the October 04, 2021 edition of Bloomberg Businessweek.
Start your 7-day Magzter GOLD free trial to access thousands of curated premium stories, and 8,500+ magazines and newspapers.
Already a subscriber? Sign In

Instagram's Founders Say It's Time for a New Social App
The rise of AI and the fall of Twitter could create opportunities for upstarts

Running in Circles
A subscription running shoe program aims to fight footwear waste
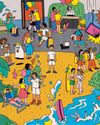
What I Learned Working at a Hawaiien Mega-Resort
Nine wild secrets from the staff at Turtle Bay, who have to manage everyone from haughty honeymooners to go-go-dancing golfers.

How Noma Will Blossom In Kyoto
The best restaurant in the world just began its second pop-up in Japan. Here's what's cooking

The Last-Mover Problem
A startup called Sennder is trying to bring an extremely tech-resistant industry into the age of apps

Tick Tock, TikTok
The US thinks the Chinese-owned social media app is a major national security risk. TikTok is running out of ways to avoid a ban

Cleaner Clothing Dye, Made From Bacteria
A UK company produces colors with less water than conventional methods and no toxic chemicals

Pumping Heat in Hamburg
The German port city plans to store hot water underground and bring it up to heat homes in the winter

Sustainability: Calamari's Climate Edge
Squid's ability to flourish in warmer waters makes it fitting for a diet for the changing environment

New Money, New Problems
In Naples, an influx of wealthy is displacing out-of-towners lower-income workers