
The new coronavirus was a test of America’s ability to protect the health of its people, and the country failed. The U.S. has the greatest number of confirmed cases and deaths in the world. Months after arriving in the U.S., the virus that wrecked the economy with disorienting velocity continues to inflict an unfathomable human toll.
The U.S. isn’t alone in failing to stop the coronavirus. But it is unique in how much of the nation’s economic resources are devoted to health care—about 18% of gross domestic product, more than any other country. The spending, approaching $4 trillion a year from taxpayers, employers, and households, is what makes America’s vulnerability to Covid-19 striking. What are we spending $4 trillion for, if not to avert disease and death?
The virus exposed some of the structural weaknesses in America’s approach to health care and health. Diagnostic tests, delayed and in short supply, were inadequate to detect the virus’s early spread. Hospitals with billions of dollars in revenue couldn’t secure dollar masks to protect staff. Local health departments charged with containing communicable diseases were quickly overwhelmed. They’re now scrambling to hire epidemiologists and contact tracers to track the pathogen as the country reopens. Neglect of public health funding has left U.S. companies playing catch-up to build the infrastructure to develop and manufacture a vaccine.
This story is from the June 15, 2020 edition of Bloomberg Businessweek.
Start your 7-day Magzter GOLD free trial to access thousands of curated premium stories, and 8,500+ magazines and newspapers.
Already a subscriber ? Sign In
This story is from the June 15, 2020 edition of Bloomberg Businessweek.
Start your 7-day Magzter GOLD free trial to access thousands of curated premium stories, and 8,500+ magazines and newspapers.
Already a subscriber? Sign In

Instagram's Founders Say It's Time for a New Social App
The rise of AI and the fall of Twitter could create opportunities for upstarts

Running in Circles
A subscription running shoe program aims to fight footwear waste
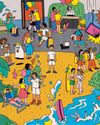
What I Learned Working at a Hawaiien Mega-Resort
Nine wild secrets from the staff at Turtle Bay, who have to manage everyone from haughty honeymooners to go-go-dancing golfers.

How Noma Will Blossom In Kyoto
The best restaurant in the world just began its second pop-up in Japan. Here's what's cooking

The Last-Mover Problem
A startup called Sennder is trying to bring an extremely tech-resistant industry into the age of apps

Tick Tock, TikTok
The US thinks the Chinese-owned social media app is a major national security risk. TikTok is running out of ways to avoid a ban

Cleaner Clothing Dye, Made From Bacteria
A UK company produces colors with less water than conventional methods and no toxic chemicals

Pumping Heat in Hamburg
The German port city plans to store hot water underground and bring it up to heat homes in the winter

Sustainability: Calamari's Climate Edge
Squid's ability to flourish in warmer waters makes it fitting for a diet for the changing environment

New Money, New Problems
In Naples, an influx of wealthy is displacing out-of-towners lower-income workers